“Never doubt that
a small group of thoughtful, committed citizens can change the world;
indeed it’s the only thing that ever has”
-Margaret Mead
Getting FASD in the DSM: The Work of a
Few Good Doctors
by Kathleen Mitchell
Over time, I have come to the conclusion that more specifically
diagnosing Fetal Alcohol Spectrum Disorders (FASD) is key to both
prevention and treatment. This is based upon my own experiences
and observations in the professional world.
The day my daughter, Karli, was diagnosed with Fetal Alcohol Syndrome
(FAS) I knew that my life had changed forever. For 15 years I had
searched to understand why she was not learning and growing stronger
like my two other children. The most common misconception that I
encountered was that Karli was going to “grow out of it.”
Physicians told me that her developmental disabilities were a result
of suffering from chronic ear infections. “Give it some time,
children are very resilient to these types of delays; she’ll
be fine,” was the message I heard over and over again.
Karli is now 32 years old. She never did grow out of it.
Once she was correctly diagnosed with FAS and I understood that
Karli’s disabilities were a direct cause of my drinking during
pregnancy, it catapulted me into advocacy. I had not known that
alcohol could cause harm to my unborn child. I knew then I had to
tell others of what had happened to Karli. I jumped in with both
feet, and shared our story with all who would listen to educate
other women. This was to become my destiny; if I could prevent one
alcohol exposed birth, then my time was well spent.
During my advocacy efforts, I met Susan Rich, who shared a similar
passion for FASD prevention. Since then, she has become a child
psychiatrist and is currently completing a two-year fellowship at
Children’s National Medical Center in Washington, D.C. Along
with Dr. Roger Peele, an American Psychiatric Association (APA)
trustee, she recently wrote and submitted an action paper that advocates
that APA explore having FASD included in DSM-IV-CR / DSM V (Diagnostic
and Statistical Manual for Mental Disorders, Book IV Content Revision
and Book V, respectively) and subsequent editions of the manual.
Dr. Kieran O'Malley of the University of Washington's Fetal Alcohol
and Drug Unit offered invaluable assistance and guidance for her
paper. I was delighted to be included in that process. We also had
brilliant input from Adam Litle, our past Director of Public Policy
at the National Organization on Fetal Alcohol Syndrome (NOFAS).
The paper was quite a success! It received a unanimous endorsement
from the Washington Psychiatric Society Board of Directors, as well
as from the Mid-Atlantic States, the APA, the American Academy on
Child and Adolescent Psychiatry's Assembly, the Area Committee on
Members-in-Training, and the APA's Assembly (at their annual meeting
in May 2005).
The importance of having a psychiatric code for FASD from infancy
to adulthood has been discussed for years. This code will open the
doors for early intervention. Currently there is no way for psychiatrists
to diagnose FASD, although they are typically the ones who treat
individuals with FASD. The majority of individuals with FASD do
not have mental retardation, but may have numerous behavioral, mental
and/or psychiatric issues that place them in the care of psychiatrists.
Psychiatrists will treat them based on symptoms and behaviors, even
when they suspect the issues are related to prenatal alcohol exposure.
Pediatric dysmorphologists typically are the medical professionals
that diagnose FAS, but may not identify other disorders associated
with prenatal alcohol exposure such as Alcohol Related Neurodevelopmental
Disorder (ARND). As well, the dysmorphologists form their diagnosis
based on the transitory appearance, from ages 6 to 12 years, of
the classic FAS facial dysmorphology. Some physicians report that
they are reluctant to diagnosis FAS because there are really no
treatments or services available, so they prefer not to “label”
children.
Obviously, failure to identify and diagnose these disorders results
in underreporting of FASD. Most health care professionals and institutions
are greatly ill informed on this issue and view it as a “rare
disorder.” NOFAS estimates that 40,000 (or 1 in 100 infants)
are born with some type of preventable damage from prenatal exposure
to alcohol. That is a population larger than those with Down syndrome,
cerebral palsy, and spina bifida combined.
There are many benefits that would naturally result from inclusion
of FASD in the DSM:
- Increased awareness of FASD among those that work in the mental
health field, such as psychiatrists, psychologists, therapists
and counselors.
- Increased global awareness of FASD in all healthcare and human
services systems of care.
- Better accuracy in the actual numbers of FASD cases treated.
- Increased motivation to intervene and treat women with addictive
disorders.
- Increased efforts to prevent FASD.
- Enhanced services for individuals with FASD.
- Increased knowledge of pharmacological and other interventions
that are successful for individuals with FASD.
Having a DSM code for FASD may result in a domino effect. The
more cases that are identified, the more healthcare professionals
would become aware of the disorders, and then the more likely they
are to understand the importance of prevention.
Certainly, individuals with FASD and their families are receiving
services; they are in our systems of care. The question becomes:
Are they receiving the correct services? As most individuals are
undiagnosed or misdiagnosed, unfortunately, the answer becomes:
Probably not. Those administering of our systems of care just do
not know what they do not know!
This is such an important advocacy effort that this committed
group of physicians has taken on. I honor Dr. Rich for her commitment
to making a difference in preventing FASD, Dr. Peele for his support
and enthusiasm, Dr. O’Malley for his brilliance, expertise
and desire to help those with FASD, and NOFAS members for having
the insight to understand the importance of supporting this effort.
As always, this is a personal effort for me, as I see it as a way
to help other families struggling to help their children.
Kathleen Mitchell is the vice president and national
spokesperson for the National Organization on Fetal Alcohol Syndrome
(NOFAS).
| Your voice
is important!
You can help this effort to include FASD in the DSM by contacting
your local Psychiatric Association, and by sending a letter
to the president of the American Psychiatric Association expressing
support for inclusion of FASD in the DSM. Dr. Susan Rich is
compiling personal stories and letters from families, researchers
and advocates to share with the committee that will be studying
the issue. If you are interested in contributing, please write
a description of the mental health issues and challenges your
family member has experienced, along with the tribulations
of not having an accurate diagnosis, and email it to Dr. Rich
at srich@cnmc.org. Please use “FASD in the DSM”
in the email’s subject heading.
|
return to top
Prenatal Alcohol Exposure Research in the
early 1900s
by Katy Jo Fox
The discovery:
I have been a member of FASlink (a ListServ for issues relating
to Fetal Alcohol Spectrum Disorders) for eight years now, and every
once in a while something will be posted that completely astounds
me. This past January was one of those times. A wonderful Canadian
gal named Claudia, doing online research into women's drinking habits
pre-1950, stumbled upon a book with a most interesting photo (see
below) introducing one of the chapters. She sent the link over FASlink
so that we too could see it.
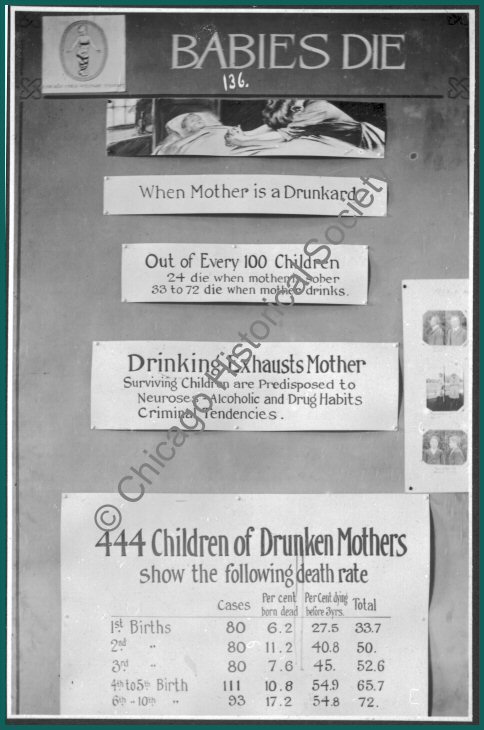
Babies Die exhibit: The Chicago Child
Welfare Exhibit; 1911. Photographer unknown.
Courtesy of the Chicago Historical Society.
My quest:
I had to know more about this photo. The credits were given to
the Chicago Historical Society (CHS), so that is where I started.
I emailed them asking for more information. While I waited for a
reply, I slowly enlarged the picture so I could somewhat make out
the first three of the four words under the logo in the upper left-hand
corner: Chicago Child Welfare. I went to Google.com to search for
that organization. The results delivered that final word: Exhibit.
I started surfing through the links and found a book titled "The
Child in the City; a Series of Papers Presented at the Conferences
Held During the Chicago Child Welfare Exhibit." Harvard had
a scanned copy of this book online, and I was thrilled to see the
logo on its front page. Some rather historical figures stood out
in the table of contents, including Jane Addams and Booker T. Washington.
Unfortunately, there was no mention of alcohol and mothers who drink
in this book. Another link told me a bit more about this exhibition—a
quarter million people attended, more than an eighth of Chicago's
population at that time.
I emailed CHS, told them what I had found, and asked for confirmation
that this photo was from the Chicago Child Welfare Exhibit. CHS
confirmed that it was, and that it is now part of a collection of
photos the society has from the exhibit. They did not know any more
about it, but did say that the exhibition took place May 11-12,
1911. They did some research and found a page showing entries for
the exhibition in the Chicago Record Herald, and mailed
me a copy of that page. Unfortunately, the clipping did not help
my quest. A few weeks later, a larger, scanned version of the picture
arrived from CHS. I enlarged it further, but was unable to read
the small writing below the three pictures on the left. However,
I could see that the first part of the word on top of those pictures
read “Feeble-M," and that the pictures were not taken
at a jail (although they looked like mug shots).
I kept searching for other angles on Google. I started at the beginning,
the online book I found the picture in, titled: “The First
Measured Century.” It is a reference volume for a 3-hour PBS
special of the same name. As I searched for the exact site, I came
across a transcript of a discussion on "Infant and Maternal
Mortality: How Julia Lathrop and the Children's Bureau Tried to
Save the Babies." Unfortunately, the Children's Bureau was
established in 1912, following the exhibit. A search on Julia Lathrop
herself amazed me. Julia lived at Hull House with Jane Addams, and
one of her jobs involved visiting over 102 almshouses, farms and
settlements in and around Chicago that collectively housed the mentally
ill, aged, sick and/or disabled. She also helped found the first
juvenile court in the United States in 1899, and even established
a psychiatric clinic for young offenders. Julia wanted to prove
that mental illness was not a sign of moral defect, a belief that
was counter to common opinion, even among those in the medical field.
Later in life, she focused her work on combating infant mortality.
Here was a wonderful woman who did all kinds of statistical research,
whose CV would have been just as long or longer than Ann Streissguth's,
FASD’s pioneering researcher, and who had all the qualifications
needed to do the kind of research seen on this picture. More importantly
for my quest, she had been doing research prior to 1911.
In my hunt for information on Julia Lathrop I came across an article
by Dr. Patrick Curtis titled, “The Beginnings of Child Welfare
Research in the United States.” It compared Julia’s
belief about the cause of mental illness to those following a different
path, specifically, eugenic reformers. They believed that so-called
moral defects, like drunkenness, were passed down to their children,
in the form of “feeble-mindedness” and delinquent behavior.
I had a hard time explaining to someone the difference between this
belief and Julia’s, especially when applied to drinking during
pregnancy, since alcohol was the teratogen that caused the damage,
and the mother was the person who actively drank it. I developed
this hypothetical scenario as a way of explanation: Say female subject
A was a “loose woman,” — definitely a moral defect
for this time period. She got pregnant and had a baby girl who,
later in life, turned to prostitution and crime. Was this just a
reflection of her environment, or was this because she was predisposed
to moral defect? Would it make a difference knowing she was prenatally
exposed to alcohol? Today we have the ability to scientifically
go out of the box. We know what alcohol does to the brain, causing
people prenatally exposed to it to be more vulnerable and making
them easy targets to the whims of criminals. Bless Julia Lathrop
for believing in something that could not then be proven!
Another source of information about the Chicago Child Welfare Exhibit
was “Childhood and Child Welfare in the Progressive Era,”
by James Marten, which had several chapters about the exhibit and
highlighted the work of Julia Lathrop. Unfortunately, the book contained
no clues about the research presented on the exhibit poster. However,
it did cite a booklet titled “The Child in the City: A Handbook
of the Child Welfare Exhibit at the Coliseum, May 11 to May 25,
1911,” published in 1911 by Blakely Printing Co. in Chicago.
Although Google could not help me track down this publication, I
was able to find and email James Marten, who told me that it was
available through Interlibrary Loan. I was quite excited when, a
few weeks later, the handbook was available at the library. Skimming
through it, I looked carefully through the names of various speakers
and committee members. No mention of Julia Lathrop. I then skimmed
through the various descriptions of demonstrations, everything from
Chicago’s Open Air School, which turned “sick school
children into stout and clever ones,” to how to sterilize
baby bottles. The descriptions were quite vivid. The previous year,
3,500 children died in Chicago from preventable diseases. One display
had a line of dolls, where every fourth doll dropped into a grave--only
three in four infants grew up. Every aspect of the child’s
life was examined, and recommendations aired.
I started to read the section titled “Eugenics,” and
by the end I knew I had found the source for this picture. It discussed
the need to scientifically look at mental and physical disabilities,
and asserted that many of these disabilities could be prevented
and that “the responsibility for these ills rests with the
parent, the community, and the state…the policy of silence
and suppression of information must be abandoned…that condemnation
and prohibition must give place to education.”
I was happy to see that it looked like the theory of eugenics was
in for a paradigm shift. Alas, it was too much to hope for. They
were only at the beginning stages of this shift. Instead of using
their knowledge to warn women about the dangers of drinking during
pregnancy, they clung to their cloak of supremacy in breeding. As
much as this quote sickens me, I have to share the last paragraph
of this section, as it completes my quest:
“Infant mortality as a result of early marriages, strong
drink, overwork and work in certain industries—the manufacturing
of lead products, for example—are shown by statistics. The
ravages of diseases are similarly set forth. A strong argument
for preventing the mating of the unfit is made by chart and photograph
illustrating the heredity of feeble-mindedness.”
Thoughts on "what went wrong":
If Iceberg readers are like me, they might be wondering why these
statistics are in archive form only. Regardless of the researchers’
personal beliefs, if they knew without a doubt that babies died
when their mothers drank (remember, there were then no resources
for keeping failure-to-thrive babies alive), and they knew that
those babies who did survive childhood grew up to have Neuroses
(depression), drug and alcohol habits, and criminal tendencies,
why was this research buried and forgotten? Perhaps it is because
with the invention of immunizations, fewer babies were dying. Perhaps
with WWI and then the Great Depression, people had other concerns
and it was slowly forgotten. Perhaps it is because the alcohol industry
found a way to suppress this information, or maybe even society
itself was in denial that a once again legal drink could have such
a harmful effect on offspring.
Interestingly enough, this question is one of the main topics in
a 2003 book titled “Conceiving Risk, Bearing Responsibility,”
by Elizabeth M. Armstrong (for those looking for a good book on
Fetal Alcohol Spectrum Disorders, I absolutely do not recommend
this book). Ms. Armstrong has a number of misguided notions (such
as Fetal Alcohol Effects being a lesser form of Fetal Alcohol Syndrome)
and the more I read her book, the more frustrated I became at her
lack of accurate and updated research, which was reflected in her
conclusion that FAS was more a diagnosis of the birth mom than brain
damage that may not even be noticed (without brain imaging, which
she also had a problem with) until adolescence. However, the first
part of this book does have an excellent historical analysis, from
Plato to the present, for those interested in the changing thought
process on the visible effects of alcohol on offspring. Again, her
ideas that these were not really a historical analysis on prenatal
alcohol exposure, more a refection on morality, may not be totally
accurate.
One bit of research mentioned in Ms. Armstrong’s book was
a study done in a Liverpool prison where William Sullivan studied
siblings of alcoholic mothers. He found that the children the mother
carried in prison, without access to alcohol, fared better than
their siblings carried out of prison. Morality could not have been
an issue in this study as the children all came from alcoholic mothers
who at one time or another spent time in prison.
Going back to the issue why this information was lost, Ms. Armstrong
does ask the question of why the research of many doctors from around
the world involving alcohol in pregnancy seemed to disappear. Her
thoughts are that, in the age of medicine and scientific research,
doctors thought that the studies of the past were not based on accurate
research. Also, after WWII, most doctors in the U.S. did not want
to accept any past research based on concepts of morality or the
supremacy of offspring. It is quite possible that she is correct,
as all other countries that had researched alcohol and pregnancy
were directly affected by Hitler’s ideology.
There are many other questions one can ask when looking into the
past. Did the research presented on the poster generate any prevention
campaigns? In Ms. Armstrong’s book there is a poster from
a 1909 anti-saloon billboard that asserts one can’t drink
liquor and have strong babies. The language in the rest of that
billboard is pretty strong and probably was viewed as more irrelevant
ranting from groups determined to close down all sources of alcohol,
rather than accurate scientific research. Was the research in this
poster seen as irrelevant ranting from people determined to better
the gene pool? We may never know the impact this poster had on those
who saw it. We may never know how far these eugenic reformers took
their research and conclusions. We may never know who exactly funded
this research and who carried it out (for those interested, the
handbook did list the names of people in the sub-committee on eugenics
for the Chicago Child Welfare Exhibit ). We can only say thank you
to those who rediscovered the harmful effects of drinking during
pregnancy – Dr. Paul Lemoine and Dr. Ken Jones (and be glad
that they did not attribute it to moral defect) – and thank
you to all who have devoted their lives to researching, diagnosing
and working with those who have Fetal Alcohol Spectrum Disorders,
as well as everyone working towards prevention.
Katy Jo
Fox is the Web master and office assistant for the Fetal Alcohol
and Drug Unit at the University of Washington in Seattle, and an
Iceberg board member.
return to top
Response to "Getting FASD in the DSM:
The Work of a Few Good Doctors"
by Charles Huffine
It was a pleasure to read Ms. Mitchell’s article and realize
once again the power of parent advocacy. I, too, have labored for
reform in the Diagnostic and Statistical Manual for Mental Disorders
(DSM) and have come to realize how slow and conservative the American
Psychiatric Association is in allowing change. My position is slightly
different than Ms. Mitchell’s.
We need to keep in mind that a psychiatric diagnosis accompanying
a medical problem needs to be separated out for inclusion in the
DSM. Fetal Alcohol Spectrum Disorders (FASD) would never be considered
a psychiatric diagnosis per se, only the brain functioning part
of that diagnosis and not the dysmorphology. I would advocate for
Alcohol-Related Neurodevelopmental Disorders (ARND) to be the psychiatric
diagnosis. Interestingly there is a possible code for ARND buried
deep in the schedule of diagnoses: DSM IV, Axis I, 310.1 Personality
Change Secondary to (X Medical Condition). The text of the DSM specifically
says that the personality change can be the difference of what the
child’s personality might have been had the child not had
damage in-utero. The medical condition is Fetal Alcohol Exposure.
This is a confusing and underused diagnosis. I have found very
few who use it even in my community where I have been advocating
for its use for many years. ARND would be a much more specific diagnosis
and would challenge the FASD community to carefully define it with
criteria that distinguishes it as a distinct diagnosis. I would
code it next to Personality Change Secondary to (X medical condition)
as 310.2.
I have earlier written for Iceberg on the importance of having
the psychiatric issues of FASD specified in the DSM as a means of
helping psychiatrists avoid throwing them into the amorphous and
much-maligned pool of Conduct Disorder and the other Disruptive
Behavior Disorders. (Huffine, C. “It’s Time Psychiatry’s
Diagnostic “Bible” Addresses FAS, Iceberg June 2000.)
I hope, in time, that this will be the case.
Charles
Huffine has practiced child and adolescent psychiatry in Seattle,
Washington since 1975. He is currently in private practice and is
the Assistant Medical Director for Child and Adolescent Services
at the King County Mental Health, Chemical Abuse and Dependency
Services Division.
return to top
What You Can Do to Support Students with
FASD
by Wendy Olson
I am a Special Education Teacher, and when asked to comment on
how to teach kids with disabilities, I often wonder what would be
helpful to others there in the trenches. Working with children who
are affected by Fetal Alcohol Spectrum Disorders (FASD) is tough.
Period. There are days when I can feel like I get little return
for my investment, as progress takes time, determination and a lot
of repetition.
Then I think of my students and how we really do have little victories
every day. Just this week, we celebrated a first 100 percent spelling
test taken by one of our students who is Fetal Alcohol Effected
(FAE). There are small and often unrecognized signs of progress.
After reminding a child with ADHD not to climb on the counters (again),
she looked up, smiled sweetly and declared fervently, “I will
learn it!” My students often humble me with their positive
outlook.
I’m a pragmatic individual. I don’t spend a lot of
time belaboring theory. Much of what I have learned comes from good,
old-fashioned trial and error. Research is important, so long as
you use it to inform your practice. In other words, what interests
me is what I can do to help my students today. What follows are
the ways I try to position my students for success.
Providing structure
I arrange my classroom with the specific needs of my student population
in mind. There should be no clutter; I avoid hanging anything from
the ceiling, and only gradually introduce the idea of displaying
student work on the back walls (usually not before January).
I break the room into areas, each with a specific function and
all visually separate from the rest of the room. For example, large
tables for group work are sectioned into individual spaces using
colorful electrical tape, which is necessary when working with children
who struggle with knowing where they are in space and therefore
tend to encroach upon others.
My students also often have problems with sensory integration,
and may be sensitive to visual, auditory or tactile input. We try
to keep the noise level down whenever possible. Turning off a few
lights and playing soft music can really help. In the past, I have
provided particularly sensitive children with construction headphones
to block out sound. But some students need input, so such a child
can hold a Koosh ball while listening to a group lesson (keeps those
busy hands from peeling the nametags off desks). Giving directions
in sign language while speaking them can give additional helpful
input to children with auditory processing issues.
When properly supported in a structured environment, even the most
profoundly affected children can learn appropriate school behaviors.
Visitors have commented that I have the best-behaved classroom in
our primary unit. When asked about what I use for a behavior management
system, I always answer, “structure.”
Structure can be applied to any activity, while allowing for choice
and freedom. When I first tried a free-choice math activity period,
we had nothing short of chaos, even though I had carefully outlined
which activities were available. So I tried upping the level of
structure by laying out each activity in a different area and placing
carpet squares where students could choose to be.
Now, before we begin an activity like this, I stop at each area,
show the activity, and ask students how many children may be in
that area. By looking at the carpet squares, they know if two or
four may play. With the simple addition of visual structure (carpet
squares), they are able to choose an activity and manage themselves
with a fair degree of independence.
Focus on the positive
While structure is key, positive behavioral management is critical.
Simply stated, you focus on the good stuff and try to give minimal
attention to the bad stuff (unless safety is an issue, of course).
The problem comes when we insist upon delivering a punishment (often
not even a natural consequence), thereby putting our attention in
the wrong direction.
It is important that we as educators remember that behavior serves
a purpose: it is communication. Before you try to stamp out a behavior,
step back and ask yourself: “Why is my student doing this?
What is the purpose?” You’ll need to teach an appropriate
replacement behavior that gets the child what he or she needs if
you wish to extinguish a problem behavior.
When thinking of recognizing the positives, praise is not enough.
There should be a reward system in place. After all, we all expect
a paycheck when we go to work and school is a child’s work.
In the best of all possible worlds, feedback is immediate and tangible.
In my room, I use classroom money that an old friend designed for
me. Our Buckaroonies are given out for hard work, good behavior
and kindness towards others. Throughout the day, my paraeducators
and I give out money to students who are on task. Children who are
not working are skipped over without comment, as we quietly tell
the other children, “Thanks for your hard work.” It
is amazing how quickly that off-task student will pick up his pencil
and get busy.
Hands-on, real life experiences are critical for children with
FASD. Students in my classroom are expected to manage their own
money. They earn additional funds by doing classroom jobs, and are
paid for these by check on the first and third Fridays of the month.
Every Friday, we have “Store” instead of math. I expect
students to sort out their cash by denomination, count it and decide
whether or not to cash their paychecks, which must be endorsed.
The store is actually a rolling set of plastic drawers with items
arranged by price. Students may purchase books, school supplies
or educational toys with the money they have earned. This is a good
opportunity to practice social skills, as children are often upset
when they can’t afford an item or someone else buys what they
had hoped to have for themselves.
Engage the students in their own education
When children are supported properly with the right degree of
structure and positive behavior management, they are ready to be
active participants in their own learning. I make a point of talking
to them about IEPs (Individual Education Plans). Whether my students
can read or not, I show them the goals that their parents and I
agreed we would work on this year. We talk about individual progress,
and familiarize them with the data sheets in their binders.
Often times, students participate in data collection by counting
the number of flashcards they read correctly, or helping to calculate
a percentage by punching numbers into a calculator (with some assistance).
I ask them to look at their scores and tell me if they did better
than yesterday. When an IEP objective is met, my students receive
a certificate to take home and get congratulations from their peers.
Educating children with FASD is a challenge, but it is also a gift;
I learn so much from my students! When structure and positive behavioral
support are provided and students are actively engaged in their
own learning, I like to think they learn from me, too.
Wendy Sunderland Olson is a Special Education Teacher
working for the Edmonds School District near Seattle, Washington.
She has a B.A. in special education and a M.Ed. in severe disabilities.
Previous to teaching, Mrs. Olson worked as a research coordinator
for the Fetal Alcohol and Drug Unit at the University of Washington.
She is currently in her fifth year of teaching in a self-contained
special education classroom serving children with FASD, Autism Spectrum
Disorders, developmental delays, and health impairments.
|

